September 22, 2025
Ventricular Standstill: Clinical Documentation and Coding Considerations
What is ventricular standstill?
- SA node is functioning, and P waves are present on EKG.
- There is no ventricular response, no contractions of the muscle.
- The presence of complete heart block with no escape rhythm.
- No cardiac output with the patient in full arrest.
- May be paroxysmal or prolonged.
Why Ventricular Standstill Is Clinically Significant
- It is a potentially fatal arrhythmia.
- The ventricles come to a complete standstill.
- Sustained for more than a few seconds, unconsciousness and no palpable pulse.
- Sustained is considered an unshockable rhythm, 10X more deadly than V-fib.
- Immediate CPR required with likely placement of a pacemaker.
Clinical Documentation Tips for Ventricular Standstill
1.) Document the Underlying Cause
- Review and query if needed for contributing factors such as:
- Electrolyte imbalances (e.g., hyperkalemia, hypokalemia)
- Drug toxicity (e.g., cocaine overdose)
- Cardiac conditions (e.g., advanced AV block)
- Non-cardiac causes (e.g., hypoxia, acidosis)
2.) Clinical Indicators
- Support the diagnosis:
- ECG findings (e.g., isolated P waves, absence of QRS)
- Symptoms (e.g., syncope, loss of consciousness, pulselessness)
- Treatment response (e.g., CPR, pacemaker insertion)
3.) Specify the Type of Block
- If applicable, clarify whether the patient has:
- Complete AV block
- Trifascicular block
- Sub-Hisian block (more life-threatening)
4.) Treatment Documentation
- Note any interventions:
- CPR
- Temporary or permanent pacemaker
- Medications (e.g., epinephrine)
5.) Avoid Ambiguity
- Review for precise terminology. Avoid vague phrases like “heart stopped” or “no rhythm” without correlating ECG or clinical context
Coding Considerations
1.) Primary Code
- I46.9 – Cardiac arrest, unspecified (Classifies as MCC when patient is discharged alive)
2.) ICD-10-CM Alphabetic Index
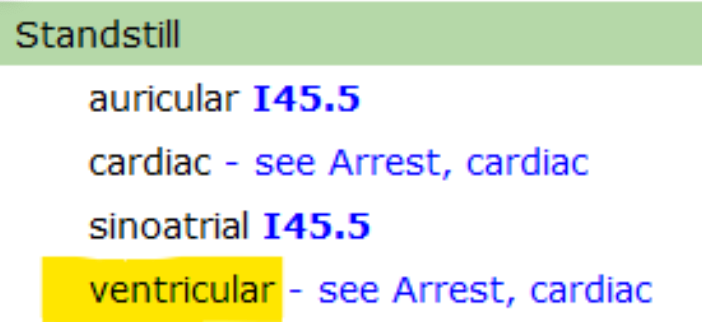
3.) Current Coding Guidance:
- When complete/3rd degree heart block is present with asystole in the instance of a brief pause of electrical conduction with spontaneous recovery of sinus rhythm, the asystole is likely caused by the complete heart block. Therefore, only I44.2 is assigned and not reported with the code for cardiac arrest.
- What does this specifically mean for CDI and Coding? It means we can't code third degree/complete heart block and ventricular standstill together.
Documentation Example:
Received page for prolonged AV block. Tele strip shows p waves with ventricular standstill for 19 seconds. Patient is asymptomatic with normal BP at time of arrhythmia. Received IV metoprolol 2.5 mg and now scheduled Q6H for PAF. No other nodal blocking agents. Electrolytes are unremarkable today. TTE was normal this admission.

Alyce Reavis, RN, MSN, CCDS, CCS
Senior CDI Educator, Consulting Services at UASI
Drawing on clinical experience in adult, pediatric, and neonatal acute care, Alyce brings valuable insight to CDI education and documentation improvement. She holds an MSN in Leadership/Education along with CCDS, CCS, and AHIMA’s outpatient CDI micro credential, supporting health systems in strengthening documentation accuracy, quality reporting, and reimbursement integrity. Passionate about truthful, clinically aligned health records, she helps organizations ensure documentation reflects true patient acuity. She is a past presenter for the ACDIS National Convention, Local chapter meetings, and the ACDIS Virtual Best Practices conference.
Works Cited
Association of Clinical Documentation Integrity Specialists & American Health Information Management Association. (2022). Guidelines for achieving a compliant query practice.
American Hospital Association. (2019). Complete heart block and asystole. Coding Clinic for ICD-10-CM/PCS, Second Quarter, 4.
Centers for Medicare & Medicaid Services. (2025). ICD-10-CM Official Guidelines for Coding and Reporting.
Available at
https://www.cms.gov/medicare/coding/icd10
ICD-10-CM Code Book. (2025).
Prutkin, J. (2024). ECG tutorial: Miscellaneous diagnoses. UpToDate.
Available at
https://www.uptodate.com/contents/ecg-tutorial-miscellaneous-diagnoses
University of New Mexico. (n.d.). Ventricular standstill.
Available at
https://www.ekgstripsearch.com/Vent_SS.htm













