August 5, 2024
Our HCC experts Nancy Koors, Vice President of Corporate Development and Mary Stanfill, MBI, RHIA, CCS, CCS-P, FAHIMA, Vice President of Consulting Services recently teamed up with Colleen White, MSM, BSN, RN, CPC, Ambulatory CDI Program Manager at ChristianaCare, for a webinar discussing Successful HCC Risk-Adjusted Programs: Tactics to Manage Your Risk-Adjusted Population. ChristianaCare is featured on the World’s Best Hospitals 2022 list by Newsweek and among America’s 50 Best Hospitals 2022 according to Healthgrades.
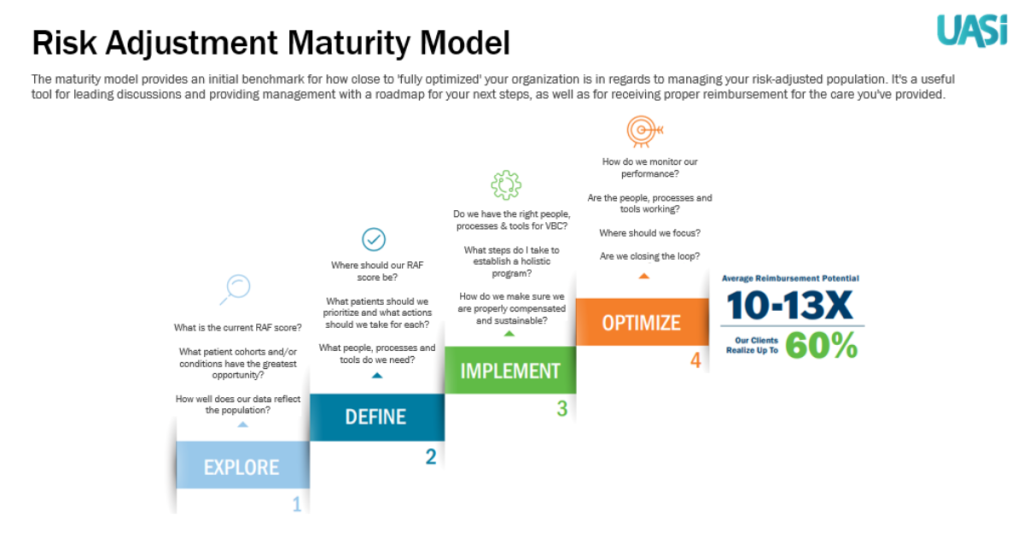
The webinar primarily focused on UASI’s Risk Adjustment Maturity Model and its four phases: Explore, Define, Implement, and Optimize, as well as lessons learned from ChristianaCare as they progressed through each phase. Here is a breakdown of each phase. Keep reading to find out in what phase your organization is.
Explore: An organization is aware that they have a growing risk-adjusted patient population, but they may or may not know how many patient lives they are managing or their RAF scores. Whether they know their RAF Scores or not, they probably realize that their scores are not a true reflection of the health of their population. There are a lot of uncertainties in this phase such as: How accurate is our documentation? How do we analyze the sheer volume of patients and visits? Where do we start? How do we prioritize? A reactive approach to the explore phase is driven by reimbursement not reflecting the care provided.
Define: The facility begins reviewing their risk adjusted patients to identify which patients do not have accurate RAF Scores. Based on this, the facility will prioritize patients for review to ensure the time spent is most productive. Typically, organizations begin to use Excel to manage the work queues. This can work early in the process, but as the patient volume increases and workflow begins to include other areas of the health system, it becomes problematic as the amount of data is difficult to manage and manual data entry becomes less reliable. The facility typically finds a chronic condition to focus on or a group of physicians to run a pilot test to determine the right people, processes, and tools needed.
Implement: The hospital has moved beyond a pilot test and begins to implement a program where consistent procedures are followed across multiple clinics or provider groups. The team typically grows and the workflow becomes the norm. A cross-training program might exist for their growing team. More sophisticated tools are sought to replace Excel.
Optimize: At this point the hospital has established a program with consistent policies and procedures. Performance is monitored, and they have been able to solve some of the easier issues such as recapturing previously identified HCCs year to year. The next step is to ensure they have captured the chronic conditions for their patients that have not been previously reported. Trends in chronic conditions will be analyzed and compared within their region. Data analytics and reporting become critical at this phase so that the health system can easily prioritize their work.
If you are interested in finding out where you are in the process of managing your risk-adjusted population, take our 3-Minute Risk Adjustment Checkup. You can also download a white paper covering insights for managing HCCs and risk-adjusted populations on our website.













