May 27, 2025
How the Mid-Revenue Cycle Impacts the Patient Experience
The Hidden Link Between Financial Workflows & Clinical Outcomes
The mid-revenue within hospitals and health systems is often viewed through a financial or operational lens, typically associated with documentation and coding workflows. When this part of the cycle becomes strained, however, the effects can extend far beyond day-to-day processes. Missed information, unclear documentation, and interruptions in data flow can influence revenue-related outcomes, quality indicators, and even how patients experience your organization.
Because this includes clinical documentation, medical coding, charge capture, and HIM, gaps within this area can affect how clinical activity is translated into administrative records. When these processes are inconsistent or disrupted, the impact becomes visible across several dimensions:
- Margin: Incomplete or inaccurate documentation can lead to under-coding, denials, or missed reimbursement.
- Compliance: Misaligned documentation can trigger payer scrutiny and administrative follow-up.
- Quality: Missing or unclear documentation can influence risk adjustment, clinical quality measures, patient safety indicators, and HCC capture.
- Trust & Experience: Documentation gaps or unclear processes can contribute to billing confusion, delays in communication, and experiences that negatively affect patient perception.
For healthcare organizations evaluating how the revenue cycle performance impacts access, accuracy, and outcomes, our mid revenue cycle solutions outline how these functions are operationally supported across the patient journey.
C-Suite Watchouts: Indicators of Revenue Cycle Strain
1. Rising Denials and Revenue Leakage
CFOs should watch for an increase in clinical denials, particularly those tied to documentation or coding issues.
2. Quality Metrics that Don’t Match Clinical Reality
CMOs should be concerned if quality outcomes (e.g., readmissions, risk scores) don’t reflect actual clinical complexity—often a result of poor documentation and HCC capture.
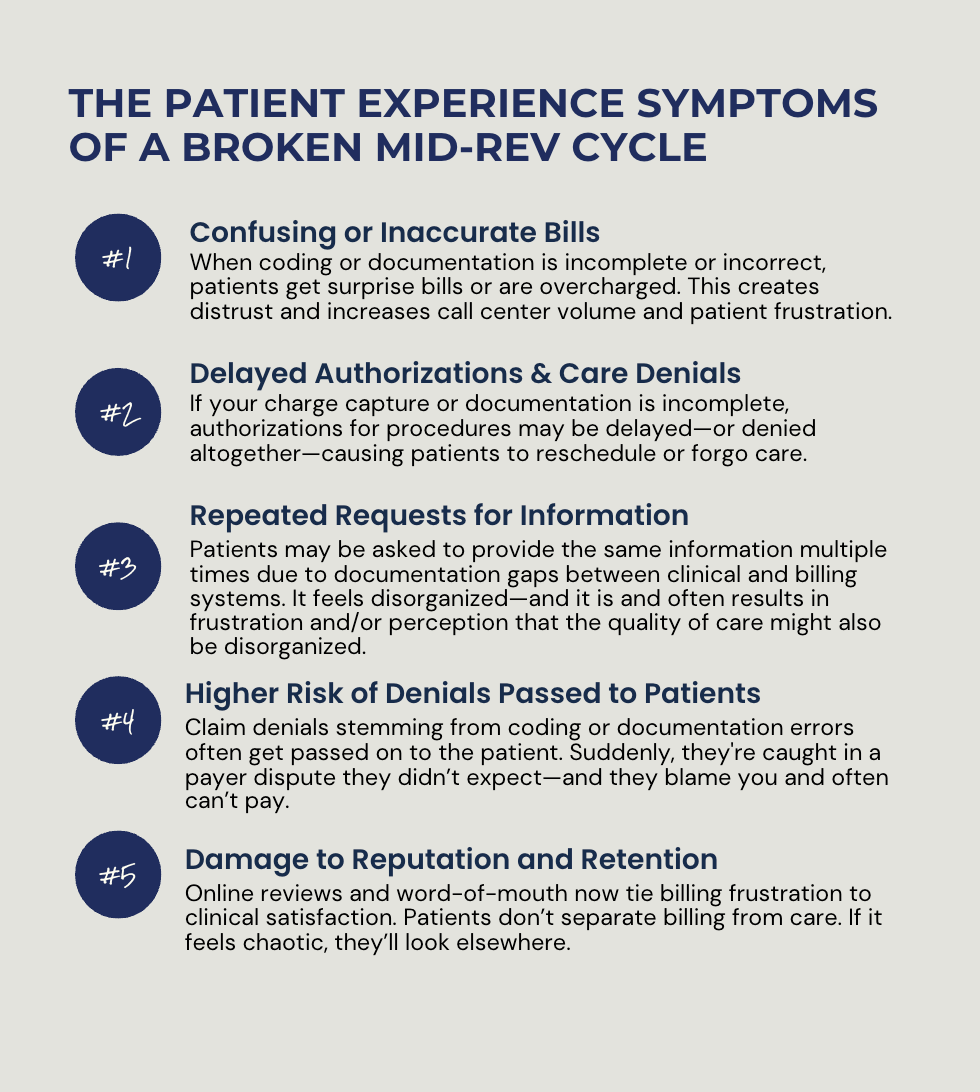
3. Patient Complaints Tied to Financial Experience
CEOs and COOs should pay attention when billing confusion or prior authorization delays become frequent drivers of patient dissatisfaction or attrition.
4. Physician Frustration with Documentation Burden & Financial Impact
CMOs may hear grumbling about clinical documentation tools or workflows. A poor CDI process creates friction with providers—lowering both morale and accuracy and impacting compensation.
Strategic Moves for C-Level Leaders to Improve the Patient’s Experience and Your Operations
CEOs:
- Treat mid-rev cycle performance as part of your patient experience and quality agenda.
- Connect revenue cycle KPIs to your broader strategy on value-based care, compliance, and growth.
CFOs:
- Invest in mid-cycle analytics to track documentation gaps and financial impact.
- Align CDI and coding with service line profitability reviews.
CMOs:
- Champion a clinical documentation culture—peer education, real-time query support, and physician-facing tools.
- Ensure alignment between EHR templates and coding needs to reduce friction.
COOs:
- Audit workflows for throughput delays or inefficiencies.
- Integrate rev cycle metrics into broader operational dashboards.













